Your Patient Safety: Resources and Information for Patients
RCSEd is committed to the global health priority of patient safety. We aim to do this by providing you, the public, with key information and resources to help you make the best of your surgical journey.
Curated by the College's Patient Safety Group (PSG), these pages will provide a wide variety of resources to support you through every step of your surgical journey, from diagnosis of conditions through to recovery.
You will find generic guides to help you optimise your hospital experience, including specific guides on asking questions, supporting vulnerable groups and consent.
You will also find links to various subspecialty organisations that will give you more information on your specific condition or type of surgery you are undergoing. This includes information on children’s surgery and dentistry.
The Surgical Journey
What to expect if you are referred to a hospital specialist
It is likely that when you are referred to see a surgeon, your appointment will take place in hospital. Hospitals can be busy, overwhelming places if you have not been before, so do arrive with plenty of time to spare, and do not be frightened to ask a member of staff if you are unsure of where your appointment will be held. Your appointment letter should have details of the department and part of the hospital where your appointment is, including who you will be seeing. If you are anxious about your appointment it may be a good idea to bring someone with you provided this is in line with the hospital’s policy.
During your appointment you will be a seen by a consultant, or a member of his or her team. There might sometimes be another health professional like a nurse, dietician or care assistant present depending on the type of clinic. Some appointments may be held virtually, but rest assured that the same high standard of care will be provided by your health professional. In these cases, it is important that you ensure you have a quiet space with a good internet connection to ensure your appointment goes as smoothly as possible.
During your consultation, your surgeon will ask questions about your health concern, will examine you, and may ask that you undergo some additional tests to give him or her more information about your condition.
Your surgeon is there to help, so if you have any questions or concerns please share them with him or her. After your appointment your surgeon may choose to see you again in a follow up appointment, list you for surgery, refer you to another specialist, or discharge you if they feel you do not need to be seen again. Your surgeon will usually write to your GP or the health professional who referred you to let them know the outcome of your appointment. You can however request a copy of that letter be sent to your home, as some people find this useful for record keeping purposes.
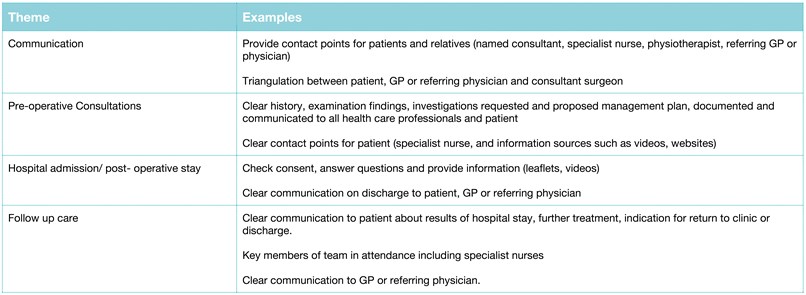
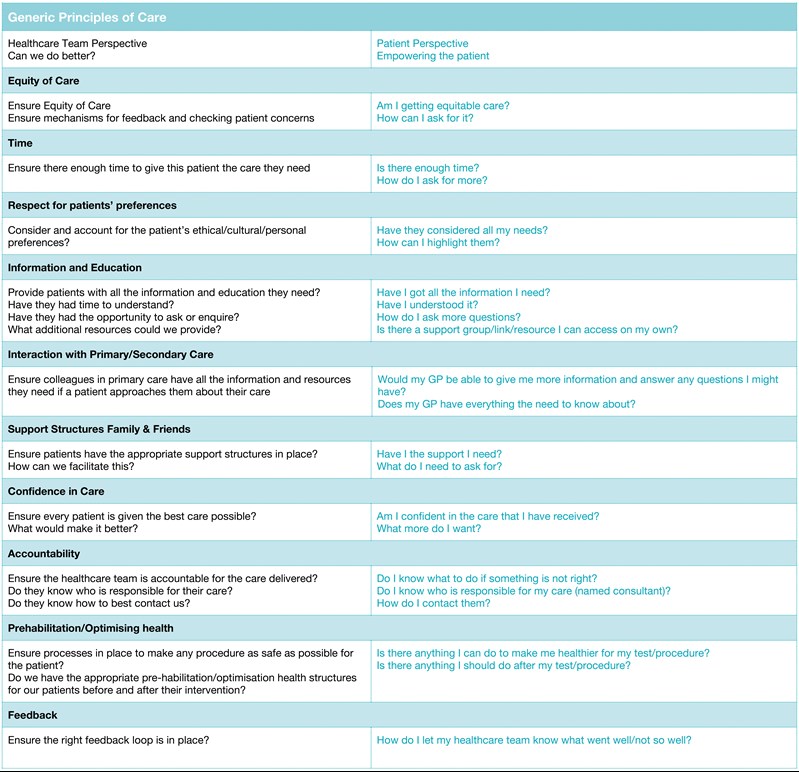
The table below highlights some important things to consider that will help you get the best out of your surgical journey.
Top Tips for Navigating Surgical Consultations
Optimising Your Patient Journey
If you get listed for a surgical procedure, it will either occur as a day-case (going home the same day) or inpatient (going home after a one or more night stay in hospital). You may get a telephone call or further appointment just before your surgery to ask some detailed questions about your health. This is called a “pre-assessment”, and is conducted by a specialist nurse or an anaesthetist. This is particularly important for people with complex conditions or health needs.
What to expect if you are having an operation
The surgical journey has many stages; this can seem challenging at times. The table below summaries some ways in which you can optimise your patient journey and make each stage of your surgical experience go as smoothly as possible.
Making Decisions About Your Care
During your surgical journey, there will be times you have to make decisions with your health professional about what is best for your health. It is important that theses decisions, whether big or small, are made with your thoughts and wishes in mind. Your health professional is there to work with you to ensure the decision you make together is one that is the safest and best for your situation. As no two patients, even ones with the same condition, are the same, it is important you have all the information you need to achieve this. You should not feel pressured to make a particular decision, or feel you have to proceed with a treatment without being comfortable that any questions you have are answered adequately.
In the medical profession, the patient is at the heart of everything we do. Two gold standard practices in every clinical encounter are shared decision making with patients, and facilitating informed consent. Below are some top tips to ensure that you come to the best decisions about your care with your clinician at every stage of your patient journey.
Top tips for making decisions about your care with your health professional
- A good consent discussion takes place in the context of a good conversation between a healthcare professional and patient. It should not be dominated by lots of direct questions from your health professional.
- You should ensure that sufficient time is given to your preferences about your life and your health priorities before making a choice about your treatment.
- Where there is treatment, there is always a choice -even if that alternative choice is no action. Before consenting to a treatment, you should understand what all your options are, even if time is short such as an emergency.
- Major treatment choices should not occur on the basis of a single conversation. If you need time to think about what is best for you, you can ask for a follow up appointment to give you the best chance of making a decision that is right for you.
- Receiving information about your treatment options is not shared decision making with your health professional. Shared decision making involves a discussion about what each options means to you.
- Medical jargon can be very confusing. It is not enough for a doctor or health care professional simply to name the complications associated with a procedure, but must be able to explain what it means in your particular situation and the chances of it happening to you.
- Your health professional must be completely open and honest in what the chances of success and failure of each treatment option for your case. This should include the option of doing nothing at all.
- Your health professional may have decision support tools or groups that may help you make the right choice in your care. Feel empowered to ask if aids such as these are available.
- You should be given the option and means to get in touch with your health professional virtually or in person if you have any further questions.
- You should not proceed with any treatment, especially if it is life changing or irreversible unless you feel this is the right choice for you.
Support for Vulnerable Patients
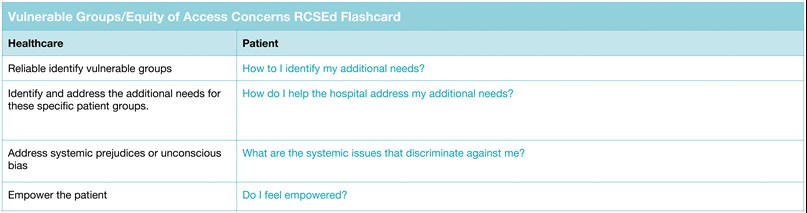
Our diverse population is made up of people who may need a bit more help that others during their surgical journey. We believe that equity of access for all is am integral part of patient safety. Disability, language or frailty should not be a barrier to accessing the care you need. If you feel that you need more help or support at any point in your journey, you should not be afraid to ask your health professional. The table below outlines some things to consider that may help you get the additional support you need.
Resources and Information on Patient Conditions
Below are links to various organisations at can give you more information on specific surgical and dental conditions